|
 |
| [ Ana Sayfa | Editörler | Danışma Kurulu | Dergi Hakkında | İçindekiler | Arşiv | Yayın Arama | Yazarlara Bilgi | E-Posta ] | |
| Fırat Tıp Dergisi | |||||||||||||
| 2017, Cilt 22, Sayı 2, Sayfa(lar) 067-070 | |||||||||||||
| [ Özet ] [ PDF ] [ Benzer Makaleler ] [ Yazara E-Posta ] [ Editöre E-Posta ] | |||||||||||||
| Can Emergency Code Team (ECT) Activation be More Effective? | |||||||||||||
| Deniz ÇEVİRME1, Ömer Faruk ŞAVLUK2, Taylan ADADEMİR1, Mustafa Emre GÜRCÜ2, Mehmet AKSÜT1, Murat Bülent RABUŞ1, Hızır Mete ALP1, Hidayet DEMİR1 | |||||||||||||
| 1Kartal Koşuyolu Yüksek İhtisas Eğitim ve Araştırma Hastanesi, Kalp ve Damar Cerrahisi Kliniği, İstanbul, Türkiye 2Kartal Koşuyolu Yüksek İhtisas Eğitim ve Araştırma Hastanesi, Anestezi ve Reanimasyon Kliniği, İstanbul, Türkiye |
|||||||||||||
| Keywords: Mavi Kod, Acil, Eğitim, Code Blue, Emergency, Education | |||||||||||||
| Summary | |||||||||||||
Objective: The Emergency Code Team (ECT) system is activated under 'Code Blue' conditions in response to urgent cases. There are many factors affecting ECT activation, including transport to the scene and the intervention applied. Both the code-giving personnel and the responding emergen-cy code teams' knowledge and experience are recognized as the two most important factors in this process. Unnecessary ECT activation wastes precious time and labour resources. For this reason, we analysed Code Blue calls and present the results herein. Material and Method: This study was performed by examining hospital data between January 2012 and September 2014. After an intervention, the team completes an emergency code form, and the data for our study were collected from these forms. All data were classified by the research team, entered into computer media and analysed. Results: The total number of Code Blue calls was 358. CPR was performed on 170 patients (47.5%), and 64 of these patients were declared exitus. The response time to the call was 1.75±0.769 min on average (1-5), and the longest response time, 5 minutes, took place in the outside of hospital and outpatient sections. Conclusion: Unnecessary ECT activation is a waste of time and labour. Placing experienced staff where/when the unnecessary code activation is primarily performed as well as conducting repeated in-service training programmes may enable more accurate ACT activation and lower the post-CPR mortality rate. |
|||||||||||||
| Introduction | |||||||||||||
Code Blue is defined as any unexpected situation, such as cardiac arrest, respiratory arrest, loss of consciousness, and lack of pulse, occurring in any section of the hospital. All hospital personnel are informed of this definition at an inservice training programme. Activation of Code Blue can be initiated by a doctor, nurse or any other nearby health personnel. Code Blue activation must reach all locations within the hospital boundaries.
Location Outside of wards: Patient registration and entrance hall, information centre, management and supportive service units. ER: Emergency room.
Outpatient: Polyclinic services, imaging centre, blood sampling, effort testing unit, and echocardiography laboratory.
Cat lab: Catheterization laboratory.
ICU: Intensive care unit.
Outside of hospital: Garden, market and car park.
In addition, the operating room and cardiovascu lar surgery intensive care unit are located inside the units. The ECT is not activated for CPR in these sections.
Activation of the team
In-service training programme
Data collection |
|||||||||||||
| Results | |||||||||||||
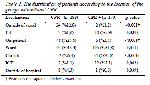
The total number of Code Blue calls was 358. CPR was performed on 170 patients (47.5%), and 64 of these patients were declared exitus. The total exitus number was 73. Nine of the patients were not resuscitated; these were intubated, terminal stage patients in the intensive care unit. The response time to the call was 1.75±0.769 min on average1-5, and the longest response time, 5 minutes, took place in the outside of hospital and outpatient sections. Arrhythmia, respiratory depression, and coronary ischaemia frequencies were statistically higher in patients on whom CPR was administered than for patients without CPR intervention (p<0.001). Frequencies of confusion, pulse weakness, and difficulty breathing were found to be statistically lower in the same group (p<0.001) (Table 1).
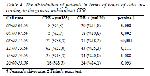
When we examined the locations of Code Blue calls, most occurred in the ward section. The farthest section of the hospital was the car park, which showed the fewest ECT activations (two patients). Among patients who received CPR, compared to non-resuscitated pa-tients, the frequencies of ward, ER, Cat lab and ICU activation were statistically higher (p=0.030; p=0.01; p<0.001 and p=0.003, respectively). Frequencies of activation outside of wards, in outpatient areas and outside of the hospital were significantly lower (p<0.001, p<0.001 and p=0.039, respectively) (Table 2).
In exitus patients, compared to surviving patients, frequencies of outside of ward and outpatient activation were statistically lower (p=0.030 and p=0.003, respectively), and the frequency of ECT activation in the ward section was statistically higher (p=0.034). There was no statistically significant difference among ER, Cat lab, ICU and outside of hospital activations (p=0.151, p=0.070, p=0.744 and p=0.213, respectively) (Table 3).
There was a statistically significant difference between resuscitated and non-resuscitated patients according to the distribution of the call time. In the resuscitated group, compared to non-resuscitated groups, the fre-quencies of calls between 00:00-03:59 and 04:00-07:59 were statistically higher and the frequency of calls between 08:00-11:59 was statistically lower (p=0.008, p=0.002 and p<0.001, respectively). For the time periods from 12:00-15:59, 16:00-19:59 and 20:00-23:59, there were no statistically significant differences in the frequency of calls (Table 4).
In the exitus group, compared to the surviving group, the frequency of emergency calls between 08:00 and 11:59 was statistically lower and the frequency of emergency calls was statistically higher between 20:00 and 23:59 (p=0.0042 and p=0.015, respectively). No statistically significant differences were observed be-tween other time groups (Table 5).
There was no statistically significant difference between resuscitated and non-resuscitated patients in terms of the distribution of days (p=0.704), seasons (p=0.091) or years (p=0.054). The exitus group, compared to the surviving group, included a larger number of patients in 2013 but a lower number in 2014 (p<0.001). No statistically significant difference was observed between groups in 2012 (p=0.541). In terms of the distribution according to days (p=0.114) and seasons (p=0.390), there was no statistically significant difference (Table 6).
|
|||||||||||||
| Discussion | |||||||||||||
For the success and effectiveness of the ECT, simply having well-educated team members is not sufficient; all hospital staff must be educated about Code Blue activation at in-service training programmes. The num-ber of non-resuscitated patients after the activation of ECT was 188, and this number exemplifies unneces-sary activation of the system. For 72 of these 188 pa-tients, the code activation took place at outpatient and outside of ward sections. After the intervention, all these patients were stable and led to polyclinic control. It is also of interest that activation at these sections was mostly performed by non-doctor health personnel due to pulse weakness, respiratory distress, and loss of consciousness. In addition, patients in these sections did not constitute a hospitalized group, which is why in-service training of the non-doctor staff in these sec-tions must be continuous. Additionally, by designing an emergency intervention room to be placed in proximity to these hospital sections, the patients can be taken to this room and examined, which may prevent unnecessary activation of the ECT. Eroğlu et al.1 investigated unnecessary activation of the ECT and found that this situation demoralizes the team. Preoper-ative preparations are organized in polyclinics, and the patients are accepted to the wards after these prepara-tions are completed in the cardiovascular surgery clinic. This is why hospitalization in the postoperative period is longer. Similarly, hospitalization after inva-sive interventions is longer in the cardiology clinic. Activation of the team that provides CPR generally takes place in wards that house this group of patients. Although it was not statistically significant, activation mostly occurred on the first days of the week; this period in particular is when patients who stay in the intensive care units over the weekend are sent to the wards. To prevent the activation of ECT in the wards, creation of an early warning control list as well as bedside monitoring of the patients who are at risk ac-cording to this list are thought to reduce unnecessary activation of the ECT2-4. For the 48 patients in the exitus group (65.8%), activation occurred from the wards, which highlights the importance of keeping the programme in the wards. When activation call time was examined, the 00:00-08:00 interval was the most intense period for CPR activation. Accurate ECT acti-vation resulting in CPR is performed in this time inter-val by the experienced and educated on-duty personnel, while activation without CPR performed is performed more often in the daytime. These activations are mostly from ward and out of ward sections, respectively, and these latter patients may be visitors of patients or conversion cases. The effect of ECT activation in the hospital on the mortality rate is controversial5,6. Nevertheless, the basic question is how to render these activations more effective. All personnel are given in-service training about CPR and ECG annually, which is provided by the quality department. All staff members who fail the exam provided with the in-service training programme must repeat the course. Additionally, the personnel completing the in-service training
programme in the wards. When activation call time was examined, the 00:00-08:00 interval was the most intense period for CPR activation. Accurate ECT acti-vation resulting in CPR is performed in this time inter-val by the experienced and educated on-duty personnel, while activation without CPR performed is performed more often in the daytime. These activations are mostly from ward and out of ward sections, respectively, and these latter patients may be visitors of patients or conversion cases. The effect of ECT activation in the hospital on the mortality rate is controversial5,6. Nevertheless, the basic question is how to render these activations more effective. All personnel are given inservice training about CPR and ECG annually, which is provided by the quality department. All staff members who fail the exam provided with the in-service training programme must repeat the course. Additionally, the CPR training programme is mandatory for all health personnel to attend at least once per year. The exitus rate increased in 2013, and no deaths were recorded after CPR intervention in 2014. |
|||||||||||||
| Conclusion | |||||||||||||
ECT activation is an effective and life-saving system. However, unnecessary activation results
in a waste of time and labour. Keeping the experienced staff where/when unnecessary code activation primari-ly occurs and repeating in-service training programmes can lower the post-CPR mortality rate. In addition, increasing the number of ward visits at the most intense hospital sections and periods of code activation, early intervention for patients who are at risk according to the control checklist, and the use of scoring systems represents feasible solutions for lowering the number of ECT activations. |
|||||||||||||
| References | |||||||||||||
1) Eroglu SE, Onur O, Urgan O, Denizbasi A, Akoglu H.Blue code: is it a real emergency? World J Emerg Med 2014; 5: 20-3.
2) McArthur-Rouse F. Critical care outreach services and early warning scoring systems: a review of the literature. J Adv Nurs 2001; 36: 696-704.
3) Mathukia C, Fan W, Vadyak K, Biege C, Krishnamurthy M.Modified Early Warning System improves patient safety and clinical outcomes in an academic community hospital. J Community Hosp Intern Med Perspect 2015; 5: 1-6.
4) Johnstone CC, Rattray J, Myers L. Physiolog-ical risk factors, early warning scoring sys-tems and organizational changes. Nurs Crit Care 2007; 12: 219-24.
|
|||||||||||||
| [ Başa Dön ] [ Özet ] [ PDF ] [ Benzer Makaleler ] [ Yazara E-Posta ] [ Editöre E-Posta ] | |||||||||||||
| [ Ana Sayfa | Editörler | Danışma Kurulu | Dergi Hakkında | İçindekiler | Arşiv | Yayın Arama | Yazarlara Bilgi | E-Posta ] |