The demographic features of patients included in our study are shown in Table
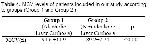
3, MCV levels of patients included in our study according to groups (Group 1 and Group 2) are shown in Table
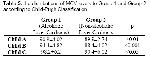
4 and the distributions of Formulas shown in Table
1 were used to calculate accuracy, sensitivity and specificity rates. MCV levels to Group 1 and Group 2 according to Child-Pugh Classification are shown in Table
5.
Click Here to Zoom |
Table 4: MCV levels of patients included in our study according to groups (Group 1 and Group 2 ) |
Click Here to Zoom |
Table 5: the distributions of MCV levels to Group 1 and Group 2 according to Child-Pugh Classification |
The study variables of patients included in our study were investigated independently from gender and age features. In our study, the MCV level of patients in Group 1 were found 94.6 ±11.9 and this was statistically significantly higher than MCV level of patients in Group 2 (p<0.001).
When the relationship between the Child-Pugh Classification and the MCV level was investigated in patients diagnosed as having ALC (Group 1), it was determined that MCV level was statistically significantly higher in Child class C patients than Child class A and B patients (respectively; p<0.001, p<0.01). Furthermore, the MCV levels of Child B and Child C class alcoholic liver cirrhosis patients were statistically significantly higher than MCV levels of patients in all Child classes (Child A, B, C) in Group 2 (p<0.001, p<0.01, p<0.01 ve4 p<0.05, p<0.01, p<0.05 respectively). Similarly, when the Child A, B, C class patients in Group 1 and Group 2 were compared among themselves no statistically significant difference was determined between Child A class patients in Group 1 and Class A patients in Group 2 in respect of MCV level (p>0.01). A statistically significant difference was determined between Child class B patients in Group 1 and Child class B patients in Group 2 and between Child class C patients in Group1 and Child class C patients in Group 2 in respect of MCV level (p<0.001, p<0.05 respectively)
Macrocytosis frequency in patients diagnosed as having ALC (Group 1) was determined statistically significantly high (20.4%, r=0.102, p<0.001) than Group 2 (3.6%).
When the relationship between the macrocytosis frequency and Child-Pugh classes was examined; it was seen that macrocytosis frequency and MCV level statistically significantly increase as the prognosis worsens according to Child-Pugh classification (By another mean, as it progresses to class C) in patients in Group 1. The macrocytosis frequency in Child class C patients was statistically significantly higher than the macrocytosis frequency in Child class A patients and Child class B patients in Group 1 (r=0.116, p<0.01, r=0.108, p<0.01 respectively).
When the patients in Group 2 were evaluated among themselves, macrocytosis was more frequent in Child class C patients (r=0.114, p<0.05). But, when the patients in Group1 and Group2 were compared in respect of the relationship between Child-Pugh classification and macrocytosis frequency, the relationship was more statistically significant in all Child class patients in Group1 than patients in Group 2 (In comparison of Child class A, B, C patients in Group 1 and Child A, B, C class patients in Group 2 r=0.112, p<0.01, r=0.204, p<0.01, r=0.106, p<0.001 respectively)
When the cut-off value was taken as 102 fl to determine the predictive value of MCV level on the prognosis, the accuracy, sensitivity and specificity rates of MCV level for the diagnosis of ALC were determined as 78 %, 93 % and 72 % respectively.



