|
 |
| [ Ana Sayfa | Editörler | Danışma Kurulu | Dergi Hakkında | İçindekiler | Arşiv | Yayın Arama | Yazarlara Bilgi | E-Posta ] | |
| Fırat Tıp Dergisi | |||||||||||||
| 2014, Cilt 19, Sayı 1, Sayfa(lar) 012-016 | |||||||||||||
| [ Özet ] [ PDF ] [ Benzer Makaleler ] [ Yazara E-Posta ] [ Editöre E-Posta ] | |||||||||||||
| Diagnostic and Therapeutic Approaches in Lung Cancer: A Single Institution Experience on 96 Patients | |||||||||||||
| Turkan DUBUS1, Bektas AKPOLAT2, Ozlem UZMAN3, Dilay DEMIRYONTAR3, Nil TOKER3 | |||||||||||||
| 1Istanbul Training and Research Hospital, Chest Surgery, Istanbul, Turkey 2Taksim Training and Research Hospital, Chest Surgery, Istanbul, Turkey 3Istanbul Training and Research Hospital, Chest Diseases, Istanbul, Turkey |
|||||||||||||
| Keywords: Lung tumor, Diagnostic methods, Surgical treatment, Akciğer tümörü, Tanı yöntemleri, Cerrahi tedavi | |||||||||||||
| Summary | |||||||||||||
Objective: To analyze the diagnostic and therapeutic approaches in lung cancer patients treated at a single institution. Material and Method: Ninety six patients with histopathologically verified lung cancer diagnosed between 2007 and 2010 were retrospectively analyzed with respect to clinical, radiological and bronchoscopic findings. Results: Male/Female ratio was 87/9, median age was 59 (45-74). Eighty two (85.4%) patients were smokers. The most frequent clinical findings were cough in 89.5%(n= 86), weight loss in 77.1%(n= 74), and phlegm in 70.8% (n= 68) of the patients. The most common findings on chest X-rays were mass in 93.7% (n= 90), mediastinal enlargement in 56.2%(n= 54), and atelectasis in 54.2%(n= 52). Histologic subtypes of the tumors were small cell lung cancers (SCLC) in 6 (6.3%), and non small cell lung cancers (NSCLC) in 90 (93.7%). Bronchoscopic and radiologic examinations revealed that the primary tumor was located in the left lung in 56 patients (58.3%). During bronchoscopy the tumoral lesions were evaluated as endobronchial in 56.2% (n= 54) and submucosal in 27.1% (n=26). The two diagnostic biopsy methods were fiberoptic bronchoscopy (FOB) and transthoracic needle biopsy (TTNB), their rates were 83.3% and 16.7% respectively. Based on the stage, SCLC patients were defined as limited in 2 patients (2.1%) and extensive stage in 4 (4.1%). NSCLC were considered operable in 41 (42.7%) patients and inoperable in 49 (51.0%). Metastases were detected in 25 patients (26.0%). Conclusion: In this study we aimed to emphasize that lung cancer operations do not necessarily require specialized centers, and in patients suitable for surgery all types of lung cancer operations can be performed successfully in any state hospital staffed by a single or a few specialists, with very low morbidity and mortality rates. |
|||||||||||||
| Introduction | |||||||||||||
Lung cancer has an increased frequency in recent years due to the increase in smoking habits, and has become the most frequent type of cancer in the World1. Lung cancer is responsible for 12.8% of cancer patients and 17.8% of cancer deaths2. The evaluation of mediastinal lymph nodes and masses is important for both diagnostic purposes and lung cancer staging. Imaging methods such as computed tomography (CT) and positron emission tomography (PET) indicate the size and metabolic activity of mediastinal nodes with a sensitivity and specificity of 57-82% in CT, and 84-89 % in PET, respectively. Bronchoscopy plays an important role in the diagnosis and staging. Endobronchial biopsy under direct visualization can provide a diagnosis in more than 90% of cases. Surgical staging by mediastinoscopy has a high sensitivity (81%) and specificity (100%)3. The aim of this study was to perform a retrospective analysis of 96 patients with mass lesions in the lung that were considered to be malignant, to evaluate these patients with respect to diagnostic and therapeutic approaches and their results, and compare them with the data in the literature. |
|||||||||||||
| Methods | |||||||||||||
This study included 96 patients hospitalized with possible diagnosis of lung tumor between October 2007 and December 2010. All patients underwent an initial physical examination, chest radiography, and computed tomography of the thorax, followed by bronchoscopic biopsy and transthoracic needle biopsy (TTNB) for histopathologic diagnosis. Bronchoscopy was performed orally using fiberoptic bronchoscopy (FOB). Histopathological types of tumors and their locations in the bronchial tree were determined. The data were analyzed with the SPSS 12 package program. Descriptive statistics were shown as the frequency and related percentage (%). A minimum of 2 and a maximum of 5 FOB biopsy samples were taken in our patients. A coagulation profile was obtained prior to the CT guided TTNB. Patients under acetyl salicylic acid treatment for comorbidities were told to discontinue treatment at least 10 days prior to the procedure. In all patients, bleeding diathesis has been ruled out. The location of the lesion was confirmed by CT. The patients were not premedicated before the procedure. The operative site was prepped with 10% Polyvinylpyrrolidone iodine (Povidoneiodine). Aspiration biopsy was performed using a 22-gauge Chiba needle and a 20 ml syringe. Aspiration material was fixed with alcohol. All patients were followed up for pneumothorax after the procedure and control chest X-rays were taken. PET CT and cranial MRI were obtained for metastatic screening in patients already diagnosed and planned to undergo surgery. Cervical mediastinoscopy was performed for staging, especially in tumors of the left lung in patients with mediastinal Fluoro Deoxy Glucose (FDG) PET uptake. The diagnosis of lung cancer was made with FOB and TTNB, and there was no need for mediastinoscopy, which was used for only staging purposes. |
|||||||||||||
| Results | |||||||||||||
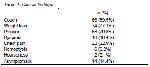
Eighty seven patients were male and 9 were female. Median age was 59 (45-74) years, 85.4% of the patients had a history of smoking. The most common clinical findings were cough in 89.5% (n= 86) of the patients, weight loss in 77.1% (n= 74), and phlegm in 70.8% (n= 68) (Table 1).
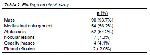
The most common chest X-ray findings were mass in 93.7% (n= 90), mediastinal widening in 56.2% (n= 54), and atelectasis in 54.2% (n= 52) (Table 2).
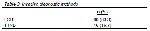
All sputum cytologies were negative in the patients. Preprocedural platelet count and prothrombin time were within normal limits for all invasive diagnostic procedures. CT-guided TTNB was performed in 16.6% (n= 16) of the patients. Eight of these were diagnosed with the first biopsy, 3 with the second, and 5 with the third. The first biopsy was diagnostic in all patients who underwent more than 3 biopsy sampling procedures. Two patients were found to have N2 positivity. Five patients developed pneumothorax, two of them required closed underwater drainage, three recovered by conservative management. Thoracic Magnetic Resonance Imaging (MRI) was obtained in 6 patients to assess the presence of vascular and vertebral invasions. The invasive diagnostic methods used were FOB (83.3%) and TTNB (16.7%) (Table 3). In our series, CT-guided TTNB was performed in 16 patients with peripheral tumors, and diagnoses were established in all. The rate of diagnosis was 50%, 68 % and 100% with the first, second and third biopsies, respectively.
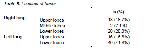
Diagnostic bronchial lavage was also performed in all patients who underwent FOB, as well as mass biopsy. Cytopathologic examination of bronchial lavage did not show any findings related to a malignancy. Initially, FOB biopsy and lavage were performed in patients with peripheral lung tumors. In histopathological examination, 6.3 % (n= 6) of 96 patients had SCLC, and 93.7 % (n= 90) had NSCLC. Among NSCLC patients, 33.3 % (n= 32) were not classified, 12.5 % (n= 12) were found to have adenocarcinoma, 39.6 % (n= 38) epidermoid carcinoma, and 8.3 % (n= 8) malignant epithelial tumors (Table 4).
Two of the patients who underwent TTNB developed hemoptysis. There was no need for surgical intervention. In 5 of the patients who underwent TTNB, two underwent tube thoracostomy, and three were given conservative treatment, these latter three patients were hospitalized and followed up with nasal oxygen support, and eventually selfimproved. Unclassified NSCLCs were consulted and confirmed with the Department of Pathology in the Medical Faculty as an external center. The inability to classify was attributed to conditions including tumor dependent necrosis, heterogeneity, and etc. or failures related to the biopsy procedure. Radiologic and bronchoscopic investigations revealed that the most common site for the tumor was the left lung, involved in 58.3% (n= 56) of the patients. This was followed by the right lower lobe in 20.8% (n= 20) and left lower lobe in 41.7% (n= 40) (Table 5).
Bronchoscopic examinations showed endobronchial tumoral lesions in 56.2% (n= 54) and submucosal tumoral lesions in 27.1% (n= 26). Sixteen patients (39.0%) underwent a preoperative mediastinocopy during the same session for staging purposes. Frozen section was N2(-) in all patients. There were no false positivities or negativities in postoperative histopathologic studies. Metastasis was ruled out by taking needle biopsies in patients with adrenal adenomas. Among SCLC patients, 2.1% (n= 2) were at borderline stage, and 4.1% (n= 4) were at late stage. In patients with NSCLC, 42.7 % (n= 41) were operable and 51.0 % (n= 49) were inoperable (Table 6). Two point one percent of patients with small cell lung cancer and 4.1% of NSCLC were accepted inoperable due to advanced stage.
Distant metastases were detected in 26.0 % (n= 25) of the patients and were most frequently located in the corpus vertebrae. Four patients with SCLC were accepted inoperable due to distant organ metastasis. Among NSCLC patients 49 were accepted inoperable, the causes were distant organ metastasis in 21, vocal cord involvement in 2, malignant pleural effusion in 2, N3(+) involvement in 12, low respiratory parameters (fev1 under 600) in 5, advanced stage leukemia in 2, severe neurologic deficit 2, poor general condition (plegic) in 2, and refusing the operation in 3. Forty one of the patients diagnosed with lung cancer underwent surgical treatment, 39 underwent lobectomy and 2 underwent pneumonectomy (intrapericardial). The left upper lobectomy (n = 12, % 29.2), left lower lobectomy, (n = 16, 39.0%), right upper lobectomy (n = 8, % 19.5), right lower lobectomy (n = 3, 7.3%), and right pneumonectomy (intrapericardial) (n = 2, % 4.8) were performed on patients together with mediastinal lymph node dissection. All patients were followed in the intensive care unit for 1 or 2 days (mean: 1.5/day) after the operation. They were then transferred to inpatient service. Thoracic drains were kept for an average of 4 days (3-8 days). Six patients sustained a dysrhythmia which was managed in the early postoperative period (14.6%). The mean length of hospital stay was 5 days (5-9 days). According to postoperative histopathological examination, the most common tumor cell type was squamous cell carcinoma (68.2%). N1 was found to be positive in 18 patients (43.9%). The majority of our patients (n: 26, 63.4%) were stage IIB (T2N1M0, T3N0M0). Adjuvant chemotherapy was performed in 5 (12.1%) of the N1 (+) patients. Follow up visits after discharge were made in the thoracic surgery clinics, every 3 months for the first year, every 6 months for the second year, and then annually. Two patients died, 2 years and 3.5 years after the operation. Median follow-up length was 36 ± 15 (11-60) months. Follow up procedures for the patients still continue.. None of the patients who were seen to have N involvement on PET studies showed any N2 positivity after pathologic examination. Six of the patients had T3 cancer, 3 of them had chest wall involvement, 2 had main bronchus involvement, and 1 had diaphragm involvement. Rib resection was carried out in the chest wall, reconstruction was not considered necessary since the defect was at the level of the scapula. In the patient with diaphragmatic involvement, dual mesh reconstruction was made after resection of the diaphragm. The two patients who had main bronchial involvement underwent pneumonectomy through an intrapericardial approach due to the central location of the tumor. There were no postoperative complications. Two patients died during the postoperative follow up period, one due to brain metastasis, and the other due to cardiac causes. |
|||||||||||||
| Discussion | |||||||||||||
The traditional diagnostic methods for lung cancer are sputum cytology, bronchoscopic sampling methods, CT guided TTNB, and surgical methods. Although bronchoscopy is the least invasive method among the diagnostic methods, the success of the diagnosis depends on the size and location of the lesion4,5. Sputum contains airway epithelial cell debris, and the morphological analysis done by sputum cytology is used in early diagnosis of lung cancer, especially in central airway tumors such as squamous cell carcinoma6. According to the literature, adenocarcinoma is first and the squamous cell cancer is second in order of frequency. In our study however, squamous cell carcinoma was the most common, and tumors which could not be classified were second. We believe that this difference was related to the 85.4% smoking rate in our patient group. Diagnostic bronchial lavage was also performed in all patients who underwent FOB, as well as mass biopsy. Cytopathologic examination of bronchial lavage did not show any findings related to a malignancy. This proves the diagnostic superiority of FOB biopsy to diagnostic bronchial lavage. We advocate that TTNB should be repeated to increase its diagnostic value. Taking a large amount of sample rather than repeating the FOB biopsy was seen to increase the diagnostic value. The diagnostic value of FOB in detecting malignancy is 75.5%8. A previous article demonstrated that although the cytologic atypia in the sputum predicts the incidence of lung cancer especially in squamous cell lung cancer, it is a late event because the relationship is stronger in samples taken during the 5 months preceding the diagnosis of lung cancer7. All sputum cytologies remained negative in our patients. Several studies reported that depending on the histological type, lung cancer can show differences in bronchoscopic evaluation with respect to location and tumor characteristics9. It has been suggested to take at least 3 samples from visible lesions. The possibility of a diagnosis decreases in peripheral lesions, whereas this ratio reaches up to 40 to 80% with fluoroscopy guided transbronchial biopsy and bronchial brushing and washing samples. Transbronchial needle aspiration increases the sensitivity of bronchoscopy in the case of submucosal spread of the tumor and external compression of the peribronchial tumor. The use of bronchoscopy with fluoroscopy, electromagnetic navigation, or endobronchial ultrasound can significantly increase the diagnostic sensitivity in peripheral lesions and especially in lymph node sampling. All of these applications are also used in the staging of lung cancer10. Lung cancer operations used to be performed only in selected centers and by experienced teams. in the past. In this study we aimed to emphasize that in patients suitable for surgery, all types of lung cancer operations can be performed successfully in any state hospital staffed by a single or a few specialists, with very low morbidity and mortality rates. |
|||||||||||||
| References | |||||||||||||
1) Spiro SG, Porter JC. Lung cancer where are we today? Current advances in staging and nonsurgical treatment. Am J Respir Crit Care Med 2002; 166: 1166-96.
2) Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin 1999; 49: 33-64.
3) Alatas F, Dundar E, Yıldırım H, Metintas M, Akdogan Ak G. Role of real-time endobronchial ultrasound-guided transbronchial needle aspiration in the diagnosis and mediastinal. Staging of Lung Cancer. J Med Sci 2012; 32: 407-14.
4) Funakoshi Y, Sawabata N, Takeda S, Okumura Y, Hayakawa M, Maeda H. Bronchoscopically undiagnosed small peripheral lung tumors. Interactive Cardiovasc Thorac Surg 2003; 2: 517-20.
5) Schreiber G, McCrory DC. Performance characteristics of different modalities for diagnosis of suspected lung cancer: summary of published evidence. Chest 2003; 123: 115-28.
6) Bolliger CT, Sutedja TG, Strausz J, Freitag L. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J 2006; 27: 1258-71.
7) Byers T, Wolf HJ, Franklin WA, Braudrick, S, Merrick, DT, Shroyer, KR. Sputum cytologic atypia predicts incident lung cancer: defining latency and histologic specificity. Cancer Epidemiol Biomarkers Prev 2008; 17: 158-62.
8) Joos L, Patuto N, Chhajed PN, Tamm M. Diagnostic yield of flexible bronchoscopy in current clinical practice. Swiss Med Wkly 2006; 136: 155-9.
|
|||||||||||||
| [ Başa Dön ] [ Özet ] [ PDF ] [ Benzer Makaleler ] [ Yazara E-Posta ] [ Editöre E-Posta ] | |||||||||||||
| [ Ana Sayfa | Editörler | Danışma Kurulu | Dergi Hakkında | İçindekiler | Arşiv | Yayın Arama | Yazarlara Bilgi | E-Posta ] |